Layered Learning
What is layered learning, and what does it look like in community-based clinical teaching settings?
What is Layered Learning?
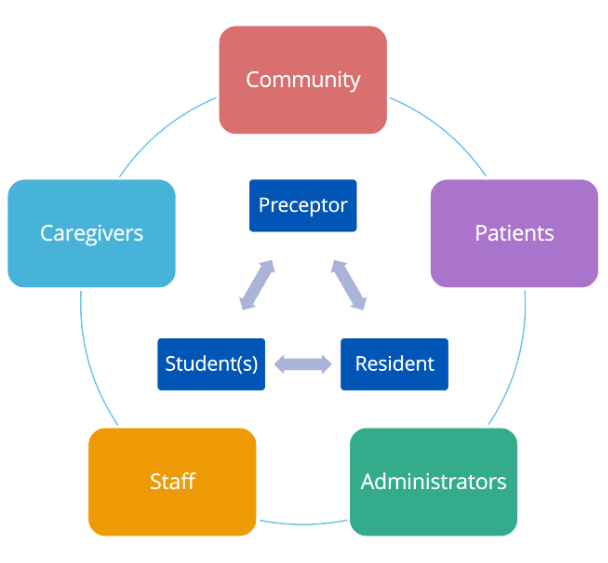
Layered learning in the medical education context refers to having multiple levels of learners and a clinical preceptor working together at the same time to teach and learn from each other.
While there is no template for how layered learning should look, we’ve spoken to patients, preceptors, residents, students, and administrators to develop the resources below to support its integration into community-based clinical teaching settings.
This project was made possible through the 2024-25 Teaching and Learning Enhancement Fund (TLEF) from the Centre for Teaching, Learning and Technology (CTLT) at UBC. Our project engaged with various community-based preceptors, patient partners, learners, and administrators from across the province of British Columbia to create resources that resonate with lived experiences.
Layered Learning Video Series

We recorded an unscripted conversation between a medical student, a resident, a preceptor, an administrator, and a patient partner, to learn their unique perspectives on layered learning. Take a look!
With our deepest gratitude, we featured (from left): Kero Daowd, Medical Student; Dr. Dan Budgell, Resident; Dr. Johnny Chang, Preceptor; Larissa McLean, Administrator; Liss Cairns, Patient Partner. Moderated by Dr. Heather Buckley.
Photo by Stephen Gillis, Illustrations by Jay White.
Resources for Preceptors

Advice from Preceptors
“Layered learning doesn’t work without investment from all parties – so it’s important to prepare everyone.”
Before Learners Arrive
Rome wasn’t built in a day – and neither are clinical teaching environments! Preparing yourself, your staff, your clinic, and your patients can go a long way in setting up your teaching for success.
Teaching Supports for New or Prospective Preceptors
The Office of Faculty Development offers a multitude of teaching resources (searchable in our resource library), but if you would prefer a more curated approach, we offer the following:
Resources for New Clinical Teaching Faculty: This page offers foundational context and resources to new clinical teaching faculty in medical education, from an overview of the medical education curriculum to educational programs for teachers. Learn more about teaching, here.
A Day in the Life of a Preceptor: Learn some general teaching principles and recommendations prior to becoming a Family Medicine preceptor, alongside a cohort of your peers. Learn more about A Day in the Life of a Preceptor.
The Teacher Certificate Program (TCP): This program aims to equip teachers in medical education with the basic knowledge and skills to teach effectively. Learn more about the TCP.
Involving the Patient as a Teacher
Layered Learning opportunities are available because patients have agreed to have learners present. As a preceptor, it is important to help prepare patients about the teaching that is taking place.
This can include:
-
- Posting signage and resident bios around the clinic to advertise that teaching is taking place (see templates in the accordion below)
- Working with your administrative staff by matching learners to patients with flexibility in their schedules, or with patients who have more straightforward visits planned (dependent on their skill level). Staff can also mention the teaching in appointment emails to patients
- Setting expectations for what the patient's role in the learning interaction will be, answering any questions they may have, and thanking them in advance for helping to develop the physicians of the future
- Providing patients with options for engaging with the teaching, and reassuring them that their care experience will not suffer for declining participation
- Consider asking the patient for feedback or suggestions to improve the teaching. And don't forget to debrief with the learner, as well!
In more rural and remote areas, you may feel that you cannot offer patients a true choice of whether they are seen by a learner. Even in those cases, it is paramount that patient consent is obtained before the learner is present. It is ultimately the patient's decision whether they are seen by learners, and providing some options for how they can engage with learners (e.g. seeing you for private matters after the student is done their tasks) may help patients feel more respected and open to seeing a learner.
Read more patient involvement tips in the FAQ section, under "My patients won't feel comfortable"!
Clinic Signage Samples
Learner Posters
Sharing a little bit of information about the learners in your clinic allows the patients to familiarize themselves prior to directly interacting with them. For longer learner placements, collaborate with your administrative staff to see if a poster about the learners would be a good fit for your clinic!
Download Resident Bio Template (Word document - Letter, 8.5" x 11")
Download Resident Bio Template (Word document - Legal, 8.5" x 14")
Teaching Clinic Signage
UBC has a plaque that you can use for your clinic to let patients know that learners may be involved in their care. Please contact Ara Silva at ara.silva@familymed.ubc.ca to request a plaque for your clinic.
Collaborating with Colleagues
Layered learning is made possible through the hard work of everyone involved, and sometimes, that may involve your colleagues who are not part of layered learning themselves. Speaking with your colleagues at your clinic and in the community before or in the early days of your learners' arrival can be very helpful.
Leaning on Experts
Your learners may arrive with specific goals that they are unlikely to meet under your supervision. For example, perhaps they want to see what labour and delivery looks like in rural areas, but that is outside your specialty. Consider reaching out to your colleagues within the clinic, or nearby, as to whether they would be willing to help out. Giving them advanced notice before the learners arrive can help streamline conversations like these.
Establishing Lines of Communication
It can be uncomfortable for learners to arrive at a clinic, especially one where many learners are present, and to witness the tension between the preceptor(s) that are eager for layered learning, and those with reservations. Some learners report that they sometimes receive or hear remarks about the large number of learners that their preceptor has taken on, and feel unwelcome.
In addition to preparing your staff and patients for the arrival of learners, we recommend speaking with your clinic colleagues and addressing their concerns about your layered learning wherever possible. It may be helpful to also express to them to bring their concerns to you, rather than your learners, to protect their psychological safety. Creating a united, supportive atmosphere can make a world of difference in the learners' feelings of safety and comfort.

Advice from Preceptors
“Adding a second learner can seem intimidating – but with the right approach, double the learners doesn’t mean double the effort on the preceptor’s part.”
Orientation of Learners
Your clinic is ready, and the learners have arrived! You’ll want to have some conversations in these early days to introduce yourself, your teaching environment, and your teaching expectations to your new learners.
We’ve gathered some helpful resources below to support those initial interactions and conversations.
How to Welcome Your Learners
Welcoming learners in a layered learning context can look slightly different from other teaching contexts. The infographic below outlines suggestions from our layered learning experts and learners.
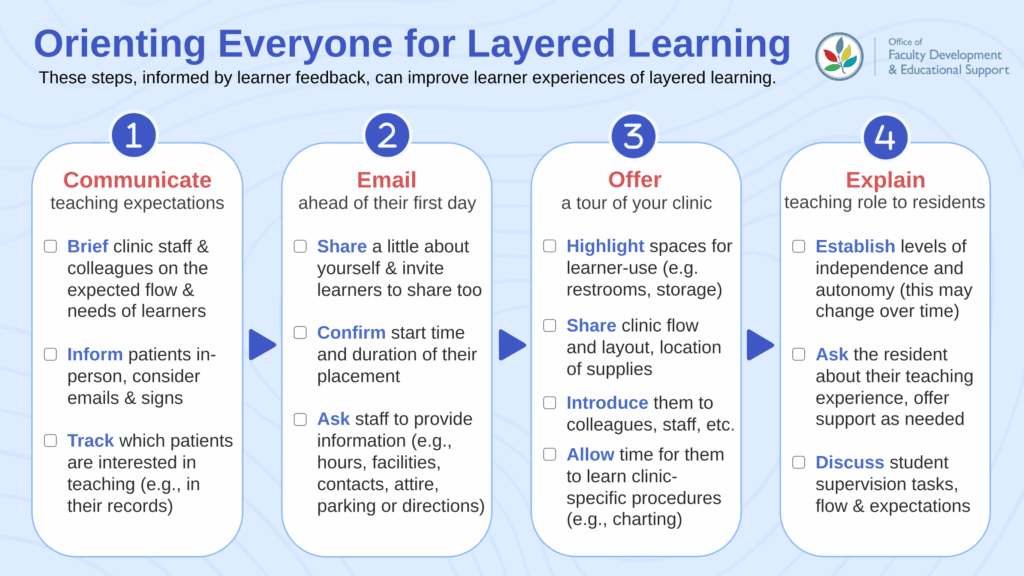
In addition to these steps, we encourage proactively communicating your commitment to provide supportive learning environments, and demonstrating it in your relationship with them.
Some ways to do this are to:
- Explain your approach to teaching through questioning, and how graded questions will work with a resident and student present
- Avoid learners against each other
- Express explicitly your openness toward feedback on your teaching
Layered Learning Primer for Learners
This resource can be emailed to learners before their arrival to allow them to understand the layered learning context that they will be learning in.
This 1-page document will:
- Briefly describe the concept of layered learning
- Outline the respective roles of the junior and senior learner
- Provide an example of a patient interaction in a layered learning environment
Explain Teaching Roles to Learners
It's important to establish a shared understanding of the teaching roles of the preceptor and the resident.
- For both residents and students:
- Clarify who the learners should approach for reviewing cases and receiving help.
- Identify which tasks can be given to align to each level of learner, to prevent misallocation of responsibilities. For example, the student may be asked to focus more on histories and physical exams, whereas the resident might focus more on differential diagnoses and treatment plans, etc.
- For the resident:
- In the beginning, discuss your expectations as a preceptor on what the resident's teaching role will be, and how teaching is done in your clinic (who sees who, when the preceptor steps in, the frequency of check-ins, etc.)
- On an ongoing basis during one-on-one check-ins, provide the resident with general advice (e.g., how to provide feedback) and/or specific guidance on how to teach a specific procedure or skill
Your check-ins with your learners are a great way to determine whether any additional explanations are needed to ensure the layered learning dynamic runs as smoothly as possible.
Scheduling Learners into Your Patient Flow
As a new preceptor in the layered learning environment, you may be wondering - how will this work, in a practical, day-to-day flow? Even with the knowledge that each learner will have unique needs that the schedule will need to accommodate, having a starting template can help visualize this flow - and get your learners started while you get to know them better.
Sample Wave Schedules Our team has consulted with experienced preceptors to give you some examples of how they schedule their learners and their various supervisory needs. These example schedules are for illustrative purposes only, and should be adapted to suit your unique learners.
For a larger view of this resource, go here!
Download the Clinic Wave Quiz (PDF) to see all schedules
Customizing Your Wave Schedules
Once you've taken some time to assess the skills of your learner(s), you will be able to adapt these schedules to meet the unique needs of your individual learners. It's also good to remember that these schedules will change over time as they become faster and more capable.
- For the resident, consider - how much supervision do they require? How often do they need to check-in with you? Do they need support or advice for supervising the medical student(s)?
- For the student(s), consider - how confident and capable are they in completing tasks? How are their interpersonal skills? Are there areas of growth to follow-up on during check-ins? Do they want or need more supervision?

Advice from Preceptors
“Trust your learners and have their back – many learners feel more confident and competent when given some room to flourish.”
During Layered Learning
Checking In with Your Learners
Layered learning is all about communication. Here are some recommendations from experienced preceptors to stay in touch with your learner's feelings, experiences, and needs.
- Check in with your learners as a group several times in the day (this may become less frequent over time as the learners often become more independent).
- Check in with your learners one-on-one once or twice a day, offering privacy and respect to your learners when offering feedback or support, and confirming that their goals and expectations are being met.
- For example, if the resident needs guidance on how to better work with the student, be sure to have that conversation without the student present.
- Engaging the resident in the assessment of the student can help support and initiate the process of a resident transitioning from a learner to a colleague.
- Model good patient interactions by making sure that the patient and all learners are included in the teaching, and asking if the patient has feedback to offer to the learner.
Read more learner check-in tips in the FAQ section, under "This will slow me down!"
Collaborative Questioning with Multiple Learners
This 3-5 minute resource is designed to help preceptors engage their learners by questioning them in a more collaborative way. For a larger view of this resource and its PDF version, go here.
Teaching Confidence and Competence - Advice for Preceptors
On Preceptor Confidence
Layered learning requires preceptors to not only teach their learners, but to trust them to teach each other, and care for patients sometimes without their direct supervision. This can be a difficult adjustment - how do you know when a learner is ready to do things on their own? What is the line between carefully guiding learners and micromanaging them?
It may take some time to accurately guage your learners' level of independence. Consider relying on some scheduling principles (like those in the section above), or pair learners with patients who have more straightforward needs while you get to know them. Over time, you will be able to assign them tasks that are tailored to their abilities and level of independence.
Preceptors should also emphasize for residents that they can ask for help and ask questions around more urgent or time-sensitive things during the clinic visit - feeling that they can rely on the preceptor can strengthen residents' confidence as a learner and a teacher.
Preceptor: "Don’t focus on perfection, but rather, experience trial and error, and working it out together instead. We need to show them that adaptability, that we're a welcoming community of professionals, and that we're all learning together. It doesn't have to be perfect. I think that that's what the thing is. And there are going to be challenges, but students are good to help work through those challenges and usually still have very positive feedback of those experiences."
Preceptor: "As a preceptor, incorporate your knowledge of what a student’s or resident’s capacity is, and what their confidence is. Reassure them that they can do it, and only step in to reorient them – step back out once they’re on course."
Preceptor: "It’s not about telling them what to do and telling them what to learn – explore through questions, and you don’t have to tell them, they will figure it out. That’s much more of a learning technique than telling them what to do."
On Learner Confidence
Preceptor: "In my clinic, I have residents observe me and take notes on my performance - this helps reinforce that we always have room for improvement, and changes the dynamic and effect of receiving feedback on learner confidence."
Resident: "My preceptor was helpful when he put specific tasks in my hands by telling me 'why don't you like go over this with [the student],' or 'why don’t you see this patient with the student.' It put me in the teaching mindset and helped me view it as like a both a teaching and a learning experience for myself."
Resident: "[Teaching the student without the preceptor present] allowed the teaching to be more informal, because it took the pressure off of both learners feeling like they had to perform in front of an authority figure."
Resident: "[The preceptor] never ever made me feel like I was like just a resident, he made me feel like I was like contributing something to like his practice. This reduced the feelings of hierarchy, reduced nervousness, and encouraged confidence."
Frequently Asked Questions (FAQ)
We hate to say it – but there aren’t many one-size-fits-all solutions.
Each layered learning environment poses its own unique challenges, and a solution that works in one clinic can be impossible in another. That said, we recognize the value of hearing from others on how common issues were addressed.
So, we spoke with those with layered learning experience about how they approached common concerns in their unique clinical teaching settings – here’s what they had to say.
What does the preceptor get out of this?
For all that layered learning is garnering attention, it may not be clear at first glance what its benefits are to the preceptor.
Here are some benefits, as highlighted by experienced layered learning preceptors.
1. Recruitment
Recruitment is a persistent challenge, especially in rural and remote areas. Giving learners an opportunity to become familiar with the community, the clinic, and its preceptors can help them consider returning to those communities in the future. Medical students also indicate that learning from near peers (i.e., residents) is important and helpful to their future career decisions.
Preceptor: "When all other avenues for recruitment had failed, I went through my contact list of my former residents, and started calling. One kindly agreed to fill a vacancy in my rural clinic, and saved us from having to close our emergency room!"
2. Mutual Learning
In layered learning, the teaching is multidirectional. This doesn't just mean that the resident teaches the student - as a preceptor, you will have opportunities to have 'aha' moments from your learners, who bring their diverse backgrounds and life experiences to the teaching interactions.
Preceptor: "Some of the residents and students would know more than I did, which was a good thing. I could empower those who knew more, whatever level of learning they were at, by acknowledging that I didn’t know [what they knew] – and that engaged the learners. [...] It helped the patients feel engaged and frankly helped me because sometimes they'd ask questions that I wouldn't have asked."
4. Fostering Teaching in the Next Generation
By modelling layered learning for learners, and inviting residents to teach students, you can normalize and coach the next generation of doctors as they learn to incorporate teaching into their everyday flow. This helps them trial their teaching skills, and can encourage them to become teachers themselves - which will contribute to the larger landscape of medical education in BC.
Resident: "I think it was good for me to have teaching experience in residency because if not, I don’t know that I would have considered taking a learner now that I’m practicing."
I don't have space for this!
Spatial constraints are one of the most common limitations that preceptors experience when looking to adopt Layered Learning. It's true - our space is exceedingly limited, there's no denying that.
Here are some ways that preceptors have made their space work.
1. Finding compromises
Using an administrative room or a private 'nook' in the clinic to take virtual calls so that the learner(s) can use the examination rooms. If you take this approach, make sure that the learner(s) know where to find you if they need you.
2. Prioritizing exam rooms
Assigning one exam room for the learner(s) to use, either independently or as a multi-learner 'team'. A past resident recommended prioritizing student use for exam rooms, and for residents to see patients in a treatment room or conduct phone visits simultaneously, if possible.
3. Coordination
Working closely with your medical office assistants (MOAs) to coordinate between your learners' program dates and goals and your upcoming appointments in your electronic medical record (EMR). Depending on how full your schedule is, it may be helpful to involve your MOAs several months ahead of the learners' arrival.
This will slow me down!
First of all, your concerns are valid.
Family medicine clinics are incredibly busy, there's no denying it. And it's important to acknowledge the work that is involved in creating a supportive learning environment, while maintaining your own wellbeing and workload. While experienced preceptors report that going from one learner to two is not double the effort once you've established a good structure for teaching, they also acknowledge that there can be a transition period in the beginning.
Preceptor: "I run a very busy practice with lots of learners. I have a family, I need to look after my own health. I can't come up with a prepar[ed] layered learning for the week. Just not gonna happen. And I don't think it's a fair expectation of preceptors to think that that's gonna happen.”
How can we manage our time while teaching learners?
Those with prior experience in layered learning recommend 'pairing up' your learners - this may be assigning a resident and student to see patients, the preceptor and resident taking a learner each, or some other configuration.
The administrative task of balancing program requirements, scheduling conflicts, and learner needs can be considerable. Working with your office staff is crucial, and showing appreciation for their work is always appreciated.
Resident: "[In our clinic,] the resident and student were picking off patients from preceptor's schedule, so there was always a lot of time and emotional space awarded to the learners, such as taking the time to do the appointment and then debrief. The preceptor was running through whoever we didn’t select at their usual pace in the meanwhile."
Preceptor: "Having the learners see patients allows me to see my daily maximum of patients. In clinics where those daily maximums are being reached without learners, I think having learners will actually help alleviate the preceptor's workload."
Below, we've outlined an example of how a day might flow with learner check-ins incorporated, based on a real resident experience.
A day with learner check-ins: A real life example
- Start of the Day: Hospital rounds, initial check-in
We would all show up at the hospital, do rounds, then resident would find preceptor and tell them which patients they would see; or the preceptor would have texted the resident earlier to say that the student would be seeing this patient, and would be debriefing with the resident.
- Later in the Morning: Checking in at the clinic, reviewing and assigning patients
Then we would all go our separate ways, and come back together at the clinic later in the morning. If the resident needed to review with the preceptor, or if the student and resident still had questions after reviewing together, this would be the time for that chat. During that time we would look at the list of patients for the day and assign who would see who, and depending on space, people would be seen in person or over a call.
By the time the resident was done, the student would be, so the resident would go see the student’s patient with them, and if additional review was needed by the preceptor, they would wait. Or if not, the resident would let the patient go (if they are of sufficient skill level, as determined by the preceptor).
- Lunchtime: Checking in about the day so far and any urgent items for review
When lunch rolls around, we would talk about how the day is going and if there were any urgent things for review.
- Afternoon: Checking in to distribute patients again
In the afternoon, we would distribute patients between the resident and student again.
- End of Day: Final check-in for review
At the end of the day, there’d be a final opportunity for review.
My patients won't feel comfortable.
We have collaborated with patient partners to ask how they feel about layered learning, and what preceptors can do for a better experience for everyone.
1. Receive Informed Consent
This can be accomplished a number of ways.
-
-
- Posting signage around the clinic to announce that teaching is taking place, and thanking patients for helping develop the physicians of the future
- Mentioning the teaching in appointment emails to patients
- Setting expectations for what the learning interaction might look like to the patient, and answering any questions they may have
- Providing patients with options for engaging with the teaching, and reassuring them that their care experience will not suffer for declining participation
-
In more rural and remote areas, you may feel that you cannot offer patients a true choice of whether they are seen by a learner. Even in those cases, it is paramount that patient consent is obtained before the learner is present. It is ultimately the patient's decision whether they are seen by learners, and providing some options for how they can engage with learners (e.g. seeing you for private matters after the student is done their tasks) may help patients feel more respected and open to seeing a learner.
The learner can also reassure the patient, as the following quote illustrates:
Patient: "The learner can reassure the patient with levity and humor, by acknowledging their nerves, stating that they know what they're doing, and explaining that they will be reviewing with the preceptor."
2. Involve Patients in the Teaching
Many patients are happy to offer feedback to the learner, or ask questions to deepen their understanding. Explaining before the learner is present what you would like patients to do will help patients to feel recognized as a participant in the learning, rather than a learning objective to be completed. Thank the patient in advance for summarizing their medical history for the learner. The preceptor and the resident can also help model good patient interactions by redirecting the patient's attention to the more junior learner present, to ensure they feel recognized and included.
Patient: "Redirect the learner's attention from asking the preceptor, to asking the patient."
Patient: "Turn your body fully to face the patient, look up from your device, and make eye contact with your patient, and thank them for coming in – it makes a difference in making the patient feel prioritized."
3. Listen to Patient Needs
Many patients have highlighted the benefits of being part of layered learning, such as having a longer visit and listening to the discussion about their care plan.
At the same time, they shared some recommendations for patient interactions:
- Care for the whole person, not just the issue at hand.
In addition to discussing treatment and care options, this may involve demonstrating your commitment to inclusive care (e.g. unlearning assumptions, sharing your name and pronouns first, etc.), or identifying support groups and other resources. - Be open and candid in explaining your thinking.
Transparency can be deeply appreciated as patients navigate their various experiences. If you're not sure why they are unwell, acknowledging that to the patient can affirm their own experience. You can also help a patient feel respected with an explanation for why you are suggesting their next steps in care. - Build a relationship.
Especially for those with chronic illnesses, seeing a different learner each visit and having to repeat their medical history each time can be frustrating and feel uncaring. While it is not always possible to brief a learner on a patient's complete history, some preparation, including avoiding suggestions they've already tried and acknowledging patient frustration can help create a better care experience.
Patient: "Great learners were those who were nonjudgemental, and who described their process in such a way where their stepping away to gain information from a preceptor did not feel like a lack of knowledge on their part."
What teaching preparations do residents receive?
All incoming residents at UBC are required to complete two modules of Residents as Teachers (RaT), a program that equips residents with the basic knowledge and skills necessary to become effective teachers.
After completing the mandatory modules, residents are encouraged to expand their teaching knowledge by attending optional sessions that explore the following teaching topics:
- Patient education
- Designing presentations for learning
- Teaching clinical reasoning
- Supporting the learner in difficulty
- Equity, diversity, and inclusion (EDI) annually rotating topic
- Teaching surgical & procedural skills
Acknowledgements
We extend our deepest gratitude to our project team, who offered us steadfast support in the creation of these resources.
-
- Drs. Meera Anand, Johnny Chang, Tara Gill, Maria Hubinette, Christie Newton, Bill Upward, Maggie Watt
- Independent Citizen-Patient and Adjunct Professor, Carolyn Canfield
- From EdTech: Stephen Gillis, Zachary Rothman
- Learners: Dr. Daniel Budgell, Aiden Wilcox
- From the Office of Faculty Development: Dr. Heather Buckley, Sharon Doucet, Minori Kato-Hopkins, Dr. Katherine Wisener
Further Reading
- Ahern, C.M., van de Mortel, T.F., Silberberg, P.L. et al. Vertically integrated shared learning models in general practice: a qualitative study. BMC Fam Pract 14, 144 (2013). https://doi.org/10.1186/1471-2296-14-144
- Morrison, T., Brown, J., Bryant, M. et al. Benefits and challenges of multi-level learner rural general practices – an interview study with learners, staff and patients. BMC Med Educ 14, 234 (2014). https://doi.org/10.1186/1472-6920-14-234
- Thomson, J.S., Anderson, K., Haesler, E. et al. The learner’s perspective in GP teaching practices with multi-level learners: a qualitative study. BMC Med Educ 14, 55 (2014). https://doi.org/10.1186/1472-6920-14-55
Do you have suggestions for topics to feature on this page?
Would you like to request a presentation on layered learning?